https://www.cas.cn/syky/202503/t20250328_5060509.shtml
http://english.cas.cn/newsroom/research_news/life/202503/t20250331_909004.shtml
https://www.cell.com/cell/abstract/S0092-8674(25)00295-8
A Chinese team has found an association between the time of stem cell infusion in allogeneic hematopoietic stem cell transplantation (allo-HSCT) and the incidence and severity of acute graft-versus-host disease (aGVHD) after transplantation. This may open a simple, easy and effective new path for clinical prevention of aGVHD after transplantation.
Allo-HSCT is a key means to cure clinical diseases such as malignant blood diseases, hematopoietic failure diseases, and congenital immunodeficiency diseases. However, even if effective immunosuppressants are used for prevention in clinical treatment, aGVHD after transplantation is still a common complication and the main cause of transplant-related deaths.
From the perspective that the recipient’s own physiological function is regulated by the circadian rhythm, the researchers explored the effect of stem cell infusion time on aGVHD through animal models and clinical cohort studies, opening up a new direction for related research. The study suggests that during allo-HSCT surgery, clinicians need to pay close attention to the potential impact of treatment time on immune-related complications and take time factors into consideration when evaluating the effect of immune-related treatment.
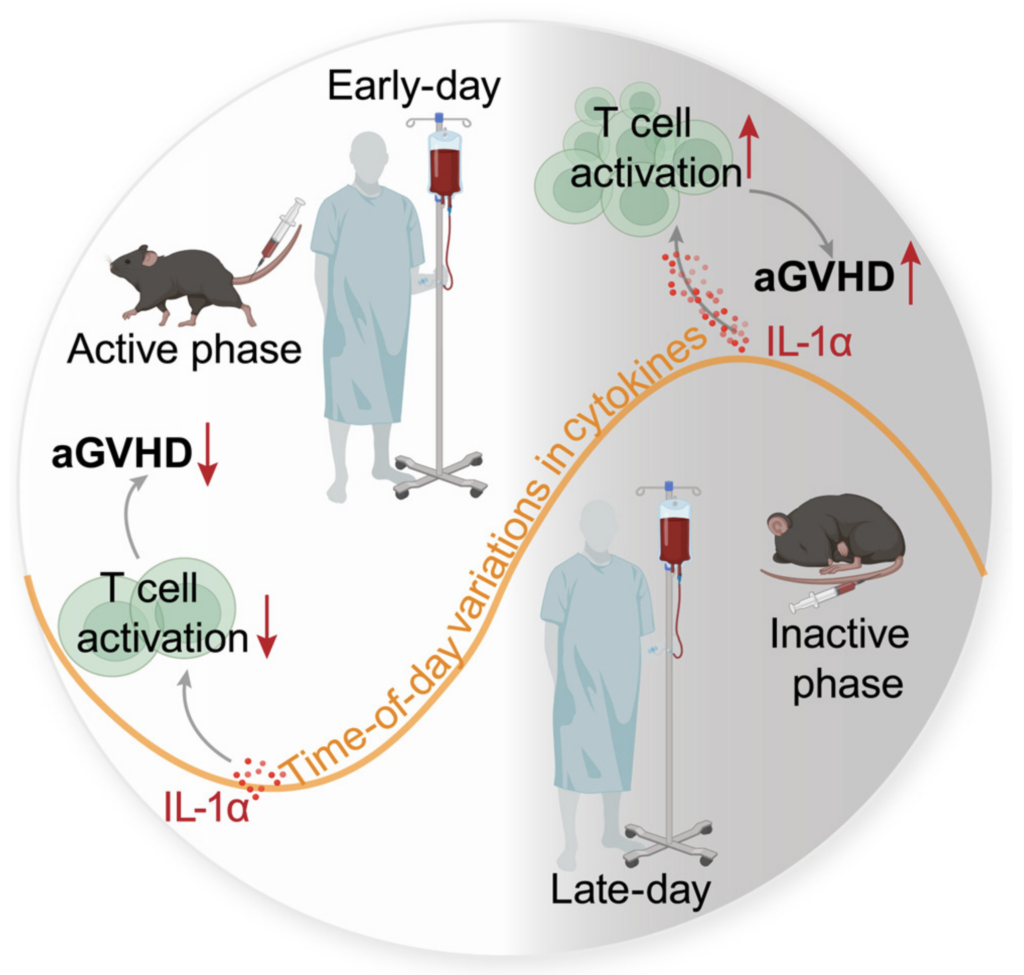
In this study, allogeneic and humanized aGVHD mouse models were constructed, and infused stem cells into mice at different times of the day. The results showed that the time of stem cell infusion significantly affected the occurrence of aGVHD, and was mainly related to the recipient’s circadian rhythm, but not to the time of stem cell collection.
The results were verified in a single-center peripheral blood hematopoietic stem cell transplantation cohort with patients grouped according to the median infusion time, which was 2 pm. To improve statistical power, the study also established a multi-center haploid transplantation verification cohort in China and reached a consistent conclusion.
To analyze the mechanism of the above phenomenon, the study detected the levels of inflammatory factors in the peripheral serum of patients and mice before transplantation. The study found that when the body just woke up (7 am for patients and ZT14 for mice), the concentrations of various cytokines and chemokines in the serum, including IL-1α, were low, and the body presented a weak pro-inflammatory environment. Cell experiments showed that the weak pro-inflammatory environment in the serum of patients just awakened before transplantation could reduce the early activation, proliferation and IFNγ secretion of donor T cells. In vivo experiments in mice also confirmed that transplantation at ZT14 could reduce T cell activation and memory T cell expression in the spleen. IL-1α, as a classic “warning factor”, can promote the activation of various immune cells including T cells. Based on the above results, the study found that the IL-1α concentration in the patient before reinfusion was positively correlated with the severity of aGVHD after transplantation. In vitro culture further verified that IL-1αcan significantly promote T cell proliferation and activation, while IL-1 receptor antagonists can inhibit T cell function. In animal experiments, the preventive use of IL-1α monoclonal antibodies can reduce the severity of aGVHD in mice in the ZT5 group. For patients who are unable to infuse stem cells as early as possible, reducing the IL-1α concentration before reinfusion may be an effective intervention to reduce the risk of aGVHD in patients at high risk.